Portal Hypertension
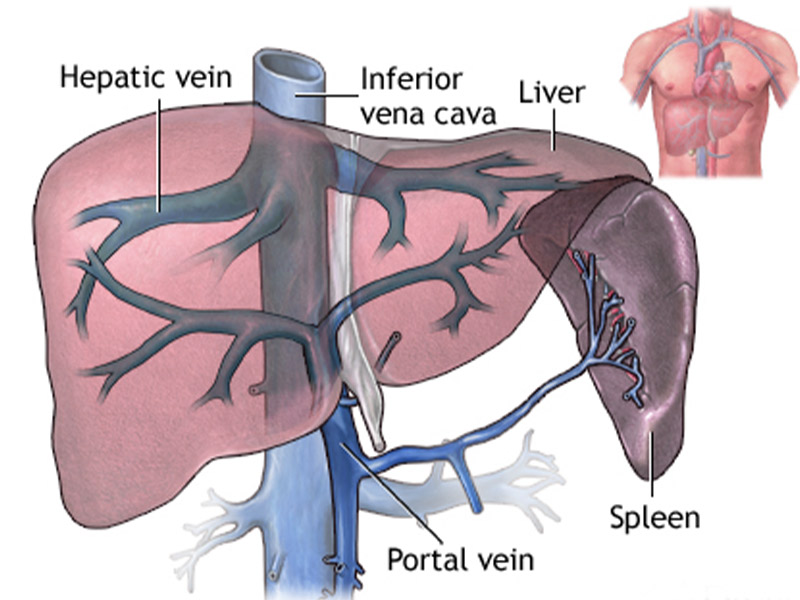
Portal hypertension is an increase in the pressure within the portal vein (the vein that carries blood from the digestive organs to the liver). The increase in pressure is caused by a blockage in the blood flow through the liver.
Increased pressure in the portal vein causes large veins (varices) to develop across the esophagus and stomach to get around the blockage. The varices become fragile and can bleed easily.
What are the Symptoms?
The onset of portal hypertension may not always be associated with specific symptoms that identify what is happening in the liver. But if you have liver disease that leads to cirrhosis, the chance of developing portal hypertension is high.
The main symptoms and complications of portal hypertension include:
- Gastrointestinal bleeding: Black, tarry stools or blood in the stools; or vomiting of blood due to the spontaneous rupture and bleeding from varices.
- Ascites: An accumulation of fluid in the abdomen.
- Encephalopathy: Confusion and forgetfulness caused by poor liver function and the diversion of blood flow away from your liver.
- Reduced levels of platelets or decreased white blood cell count.
What are the Causes?
The most common cause of portal hypertension is cirrhosis, or scarring of the liver. Cirrhosis results from the healing of a liver injury caused by hepatitis, alcohol abuse or other causes of liver damage. In cirrhosis, the scar tissue blocks the flow of blood through the liver and slows its processing functions.
Other causes of portal hypertension include blood clots in the portal vein, blockages of the veins that carry the blood from the liver to the heart, a parasitic infection called schistosomiasis, and focal nodular hyperplasia, a disease seen in people infected with HIV, the virus that may lead to AIDS. Sometimes the cause is unknown.
How is it Diagnosed?
Endoscopic examination, X-ray studies, and lab tests can confirm that you have variceal bleeding. Further treatment is necessary to reduce the risk of recurrent bleeding.
You will have the following tests to determine the extent and severity of your portal hypertension:
- Evaluation of your medical history.
- A physical examination.
- Blood tests.
- Angiogram.
- Ultrasound.
- Endoscopy.
What are the Risk Factor?
People at an increased risk for cirrhosis are at an increased risk for portal hypertension. If you have a long history of alcohol abuse, you face a higher risk of cirrhosis. You’re at a higher risk of hepatitis if any of the following apply to you:
- You use needles to inject drugs.
- You received tattoos or piercings in unsanitary conditions.
- You work in a place where you may have had contact with infected needles or infected blood.
- You received a blood transfusion before 1992.
- Your mother had hepatitis.
- You have unprotected sex with multiple partners.
How is it Treated?
- Improving your diet
- Avoiding alcohol consumption
- Exercising regularly
- Quitting smoking if you smoke
- Medications such as beta-blockers are also important to help reduce your blood pressure and relax your blood vessels. Other medications, such as propranolol and isosorbide, may help lower the pressure in the portal vein, too. They can also reduce the risk of more internal bleeding.