Irritable Bowel Syndrome (IBS)
It is a common disorder that affects the large intestine. Although not life threatening, IBS can lead to other colon related disorders such as Ulcerative Colitis, Crohn’s Disease or Colon Cancer. IBS is also known as irritable colon, mucous colitis and spastic colitis. IBS is a chronic condition that you’ll need to manage long term.
What are the Symptoms?
Symptoms of IBS differ from one person to another in terms of severity & duration. Symptoms generally tend to last for a minimum of 3 months occurring at least 3 days per month.
- Diarrhea
- Constipation
- Cramps in the abdomen, which tend to get worse after meals & are reduced after a bowel movement
- Gas or Bloating
- People with IBS may also have episodes of both diarrhoea & constipation.
- Women tend to present more symptoms around the time of menstruation. Menopausal women have fewer symptoms.
What are the Causes?
The precise cause of IBS isn’t known. Factors that appear to play a role include:
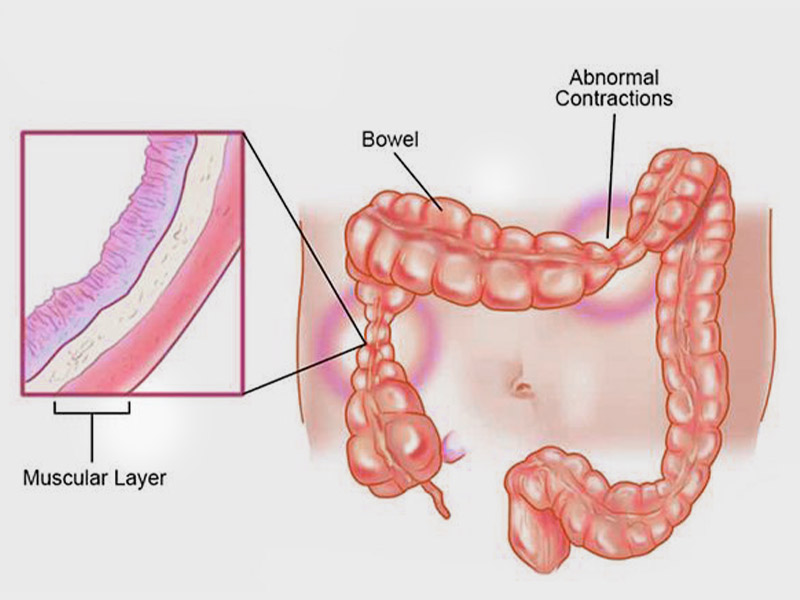
- Muscle contractions in the intestine: The walls of the intestines are lined with layers of muscle that contract as they move food through your digestive tract. Contractions that are stronger and last longer than normal can cause gas, bloating and diarrhea. Weak intestinal contractions can slow food passage and lead to hard, dry stools.
- Nervous system: Abnormalities in the nerves in your digestive system may cause you to experience greater than normal discomfort when your abdomen stretches from gas or stool. Poorly coordinated signals between the brain and the intestines can cause your body to overreact to changes that normally occur in the digestive process, resulting in pain, diarrhea or constipation.
- Severe infection: IBS can develop after a severe bout of diarrhea (gastroenteritis) caused by bacteria or a virus. IBS might also be associated with a surplus of bacteria in the intestines (bacterial overgrowth).
- Early life stress: People exposed to stressful events, especially in childhood, tend to have more symptoms of IBS.
- Changes in gut microbes: Examples include changes in bacteria, fungi and viruses, which normally reside in the intestines and play a key role in health. Research indicates that the microbes in people with IBS might differ from those in healthy people.
How is it Diagnosed?
The following tests may be recommended to diagnose Irritable Bowel Syndrome:
- Flexible Sigmoidoscopy or Colonoscopy
- Upper Endoscopy
- X Rays
- Blood Tests
- Stool Tests
- Tests for lactose intolerance, gluten allergy or celiac disease
What are the Risk Factor?
Many people have occasional signs and symptoms of IBS. But you’re more likely to have the syndrome if you:
- Are young: IBS occurs more frequently in people under age 50.
- Are female. In the United States, IBS is more common among women. Estrogen therapy before or after menopause also is a risk factor for IBS.
- Have a family history of IBS. Genes may play a role, as may shared factors in a family’s environment or a combination of genes and environment.
- Have anxiety, depression or other mental health issues. A history of sexual, physical or emotional abuse also might be a risk factor.
In addition, IBS is associated with:
- Poor quality of life: Many people with moderate to severe IBS report poor quality of life. Research indicates that people with IBS miss three times as many days from work as do those without bowel symptoms.
- Mood disorders: Experiencing the signs and symptoms of IBS can lead to depression or anxiety. Depression and anxiety also can make IBS worse.
How is it Treated?
IBS treatment focuses on relieving symptoms. Certain lifestyle modifications such as the following can help:
- Avoid foods that trigger your symptoms
- Eat foods rich in fibre
- Drink lots of fluids
- Have an exercise routine
- Get enough sleep
- Avoid foods that cause gas or bloating
- Avoid gluten
Apart from lifestyle changes, your doctor may recommend the following medications based on your symptoms:
- Fibre Supplements
- Laxatives
- Anti diarrhoea medications
- Antidepressants
- Pain medications