Hiatus Hernia
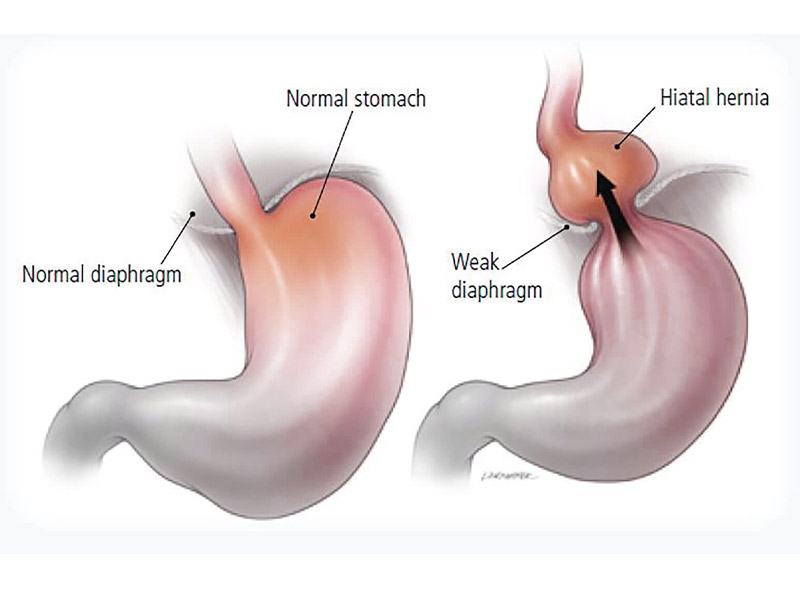
Hiatal Hernia is a condition in which the top part of the stomach protrudes through the diaphragm & into the chest region. Diaphragm is a muscle that divides the lungs from the abdomen and helps in breathing.
In most cases, Hiatal Hernias are small and may not cause any problems. However, if the hernia is a larger, it could lead to the entire stomach & other organs sliding up into the chest cavitY.
Hiatus Hernia is of two main types. These are Sliding Hiatus Hernia & Rolling Hiatus Hernia.
- Sliding Hiatus Hernia: This is when a part of the stomach & gastro-esophageal junction slide up into the chest cavity. It is the common type of Hiatal Hernia & is especially seen in women above 50 years of age, people who are overweight & long term smokers.
- Rolling Hiatus Hernia:This condition, also known as para-esophageal hiatus hernia, causes a part of the stomach to protrude into the chest cavity. In this case, the gastro-esphageal junction remains where it should be.
What are the Symptoms?
Hiatal Hernias generally do not cause any signs or symptoms. However following are some of the symptoms of Sliding Hiatus Hernia
- Burping
- Heartburn
- Nausea
- Vomiting
- Regurgitation into Oesophagus
Rolling Hiatus Hernia can cause more severe symptoms, which include:
- Abdominal or chest pain
- Abdominal bleeding
- Trouble swallowing
- Shortness of breath or trouble breathing
- Acid reflux
- Regurgitation
What are the Causes?
A hiatal hernia occurs when weakened muscle tissue allows your stomach to bulge up through your diaphragm. It’s not always clear why this happens. But a hiatal hernia might be caused by:
- Age-related changes in your diaphragm
- Injury to the area, for example, after trauma or certain types of surgery
- Being born with an unusually large hiatus
- Persistent and intense pressure on the surrounding muscles, such as while coughing, vomiting, straining during a bowel movement, exercising or lifting heavy objects
How is it Diagnosed?
A hiatal hernia is often discovered during a test or procedure to determine the cause of heartburn or chest or upper abdominal pain. These tests or procedures include:
- X-ray of your upper digestive system: X-rays are taken after you drink a chalky liquid that coats and fills the inside lining of your digestive tract. The coating allows your doctor to see a silhouette of your esophagus, stomach and upper intestine.
- Upper endoscopy: Your doctor inserts a thin, flexible tube equipped with a light and camera (endoscope) down your throat, to examine the inside of your esophagus and stomach and check for inflammation.
- Esophageal manometry: This test measures the rhythmic muscle contractions in your esophagus when you swallow. Esophageal manometry also measures the coordination and force exerted by the muscles of your esophagus.
What are the Risk Factor?
There are a few lifestyle risk factors that increase your chances of having a hiatal hernia. For many of these risk factors, the link to hiatal hernia is well established, but the cause remains unclear.
- Obesity: Obesity is one of the biggest risk factors for hiatal hernia. This may be due to increased pressure on the diaphragm due to heavy weight.
Heavy lifting: It is believed that heavy lifting puts stress on the diaphragmatic muscle, increasing the chances of an enlarged hole that allows the stomach to protrude above the diaphragm. - Coughing: The abdominal pressure caused by coughing can allow or cause the stomach to squeeze through the diaphragm.
- Straining: Straining may increase the chances of having a hiatal hernia due to excess pressure on the diaphragm. This includes straining for a bowel movement.
- Pregnancy: The abdominal pressure and hormonal changes of pregnancy can increase the chances of a hiatal hernia.
- Smoking: Smoking weakens the muscles of the diaphragm, allowing the stomach to protrude above the diaphragm.
How is it Treated?
In most cases, Hiatal Hernia may not require any treatment at all. If it is associated with symptoms such as heart burn, certain lifestyle changes such as the following can help.
Lifestyle Changes:
- Weight loss
- Avoid tight clothing or anything else that causes pressure on the stomach
- Aim to quit tobacco, if you are a smoker.
- Cut down on alcohol consumption
Avoid eating dinner too close to bedtime - Have frequent small meals
Medications
If lifestyle modifications are not helpful enough, your gastroenterologist may recommend antacids or proton pump inhibitors. Consult your doctor to know which medications can help ease your symptoms of indigestion or heart burn.
Surgical Intervention
If other treatment methods prove to be ineffective, your doctor may advise you to go ahead with a surgery. There are three ways it can be done.
- Open Surgery
- Laparoscopic Surgery
- Endoluminal Fundoplication