Piles
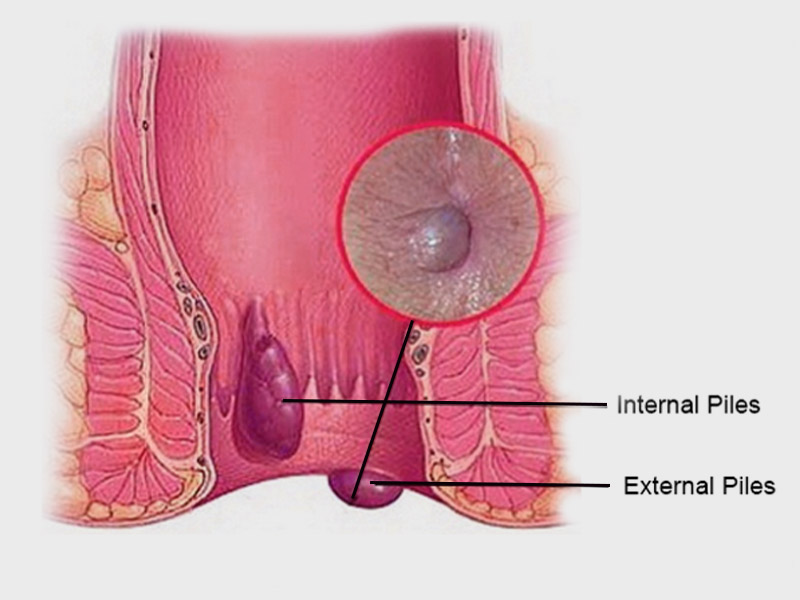
Piles is another term for hemorrhoids. Piles are the result of swollen veins in the lower anus and rectum. They can cause tissue growths in and around the anus and can lead to significant discomfort. These growths can vary in size and location.
What are the Symptoms?
- Painful lumps in and around the anus
- Itching and discomfort around the anus
- Discomfort during and after passing stools
- Bloody stools
- Excessive anal bleeding, possibly leading to anemia
- Infection
- Fecal incontinence
- Anal fistula
- Strangulated hemorrhoid, in which anal muscles cut off blood supply to the hemorrhoid
What are the Causes?
Piles result from increased pressure in the lower rectum.
The blood vessels around the anus and the rectum will stretch under pressure and may swell or bulge, forming piles. This may be due to:
- Chronic constipation
- Chronic diarrhea
- lifting heavy weights
- Straining when passing a stool
How is it Diagnosed?
- Do any close relatives have piles?
- Has there been any blood or mucus in the stools?
- Has there been any recent weight loss?
- Have bowel movements changed recently?
- What color are the stools?
What are the Risk Factor?
Certain factors may increase a person’s risk of developing piles, including:
- Pregnancy: Up to 50% of people experience hemorrhoids during pregnancy. This is due to increased pressure on the pelvis, a person having a higher blood volume, and a higher incidence of constipation.
- Age: Piles are more common in older adults. Around half of people over the age of 50 develop piles.
- Weight: Research suggests that being overweight may increase a person’s chance of developing piles.
- Diet: Eating a diet low in fiber may increase the likelihood of a person having piles.
How is it Treated?
In most cases, piles resolve on their own without the need for any treatment. However, some treatments can help significantly reduce the discomfort and itching that many people experience with piles.
Lifestyle changes
A doctor will initially recommend some lifestyle changes to manage piles.
Piles can occur due to straining during bowel movements. Excessive straining is the result of constipation. A change in diet can help keep the stools regular and soft. This involves eating more fiber, such as fruit and vegetables, or primarily eating bran-based breakfast cereals.
A doctor may also advise the person with piles to increase their water consumption. Losing weight may help reduce the incidence and severity of piles.
To prevent piles, doctors also advise exercising and avoiding straining to pass stools. Exercising is one of the main therapies for piles.
Medications
Several medicinal options are available to make symptoms more manageable for an individual with piles:
- Pain relievers: Over-the-counter pain relievers such as aspirin and ibuprofen can reduce discomfort.
- Stool softeners: Stool softeners and laxatives can make passing stools easier, which can reduce pain from piles.
- Corticosteroids: Corticosteroid creams and ointment can reduce inflammation, pain, and itching.
Surgical options
If a person has severe prolapsed piles or internal piles that are bleeding, surgery may be necessary. Surgical procedures for piles include:
- Banding: The doctor places an elastic band around the base of the pile, cutting off its blood supply. The hemorrhoid will typically fall off within a weekTrusted Source.
- Sclerotherapy: A doctor will inject medicine into the hemorrhoid to make it shrink and eventually shrivel up. This is effective for grade II and III hemorrhoids and is an alternative to banding.
- Infrared coagulation: During this procedure, a surgeon will use an infrared light device to burn the hemorrhoid tissue.
- Hemorrhoidectomy: This type of surgery involves the total removal of hemorrhoid tissue. It is the most effective option for completely removing piles, but there is a risk of complications, including difficulties with passing stools.
- Hemorrhoid stapling: During this procedure, a surgeon will use staples to block blood flow to the hemorrhoid tissue.