Barrett’s esophagus
Barrett’s esophagus is a condition in which the cells that make up your esophagus begin to look like the cells that make up your intestines. This often happens when cells are damaged by exposure to acid from the stomach.
This condition often develops after years of experiencing gastroesophageal reflux (GERD). In some cases, Barrett’s esophagus can develop into esophageal cancer.
What are the Symptoms?
Barrett’s esophagus does not cause symptoms. But you can watch for signs of the conditions it’s associated with — heartburn and acid regurgitation.
Symptoms to watch for include:
- Heartburn that worsens or wakes you from sleep.
- Painful or difficult swallowing.
- Sensation of food stuck in your esophagus.
- Constant sore throat, sour taste in your mouth or bad breath.
- Unintentional weight loss.
- Blood in stool.
- Vomiting.
What are the Causes?
The exact cause of Barrett’s esophagus is not yet known. However, the condition is most often seen in people with GERD.
GERD occurs when the muscles at the bottom of the esophagus do not work properly. The weakened muscles won’t prevent food and acid from coming back up into the esophagus.
It’s believed that the cells in the esophagus can become abnormal with long-term exposure to stomach acid. Barrett’s esophagus can develop without GERD, but patients with GERD are 3 to 5 times more likely to develop Barrett’s esophagus.
How is it Diagnosed?
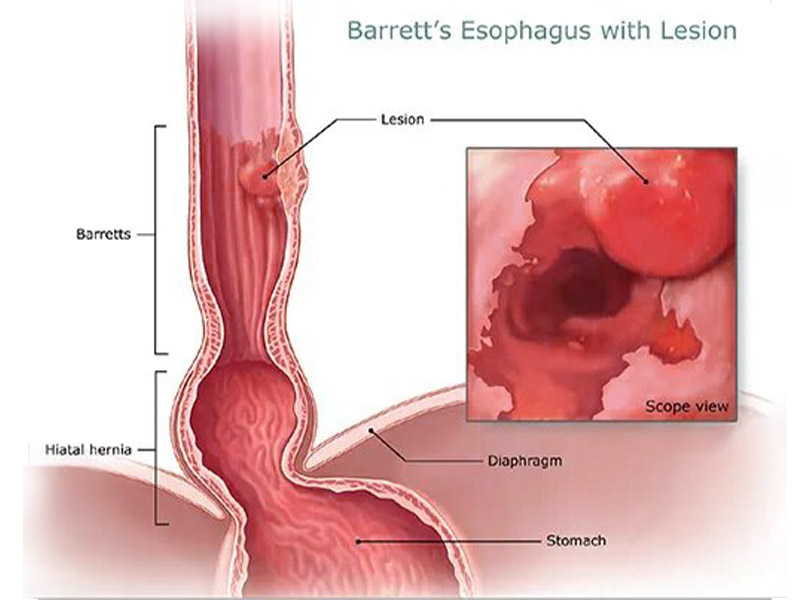
- The only way to confirm the diagnosis of Barrett’s esophagus is with a test called an upper endoscopy.
- Your doctor will be checking to make sure that your esophagus looks pink and shiny. People who have Barrett’s esophagus often have an esophagus that looks red and velvety.
- Your doctor may also take a tissue sample that will allow them to understand what changes are going on in your esophagus. A pathologist will examine the tissue to make the diagnosis.
What are the Risk Factor?
If you have GERD symptoms for longer than 10 years, you have an increased risk of developing Barrett’s esophagus.
Other risk factors for developing Barrett’s esophagus include:
- Being male
- Being Caucasian
- Being over the age of 50
- Having H pylori gastritis
- Smoking
- Being obese
How is it Treated?
Lifestyle and dietary changes:
Dietary and lifestyle changes are the first steps in treating Barrett’s esophagus. Certain foods make the reflux worse.Medication:
There are two categories of medicines for reflux. One decreases the level of acid in your stomach, and one increases the level of motility (movement) in the upper gastrointestinal tract. H2-receptor Antagonists, Prokinetic Agents and Proton pump inhibitors.Surgery:
If you did not find relief from your symptoms from lifestyle changes or drug therapy, then you may be a candidate for surgery.- Nissen fundoplication- This surgery attempts to strengthen the lower esophageal sphincter (LES) by wrapping the top of your stomach around the outside of the LES.
- Stretta procedure- A doctor performs the Stretta procedure with an endoscope. Radio waves are used to cause changes in the muscles of the esophagus near where it joins the stomach. The technique strengthens the muscles and decreases reflux of the stomach contents.
- Radiofrequency ablation- This procedure uses an endoscope with a special attachment that emits heat. The heat kills abnormal cells.
- Cryotherapy- In this procedure, an endoscope dispenses cold gas or liquid that freeze the abnormal cells. The cells are allowed to thaw, and then are frozen again. This process is repeated until the cells die.
- Photodynamic therapy- Your doctor will inject you with a light-sensitive chemical called porfimer (Photofrin). An endoscopy will be scheduled 24 to 72 hours after the injection. During the endoscopy, a laser will activate the chemical and kill the abnormal cells.