Alcoholic Liver Disease
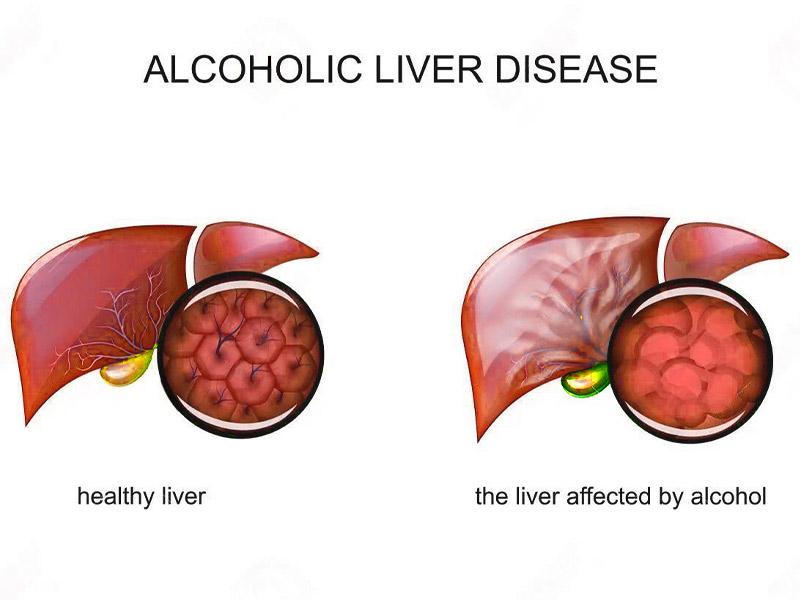
Alcoholic Liver Disease is an acute form of liver damage resulting from excessive alcohol consumption over prolonged periods of time.
Liver generally tends to regenerate & repair itself. Hence, any damage to the liver is difficult to diagnose in the early stages and by the time the damage is recognised, it is irreversible.
There are 3 types. Many heavy drinkers progress through these 3 types over time:
- Fatty liver: Fatty liver is the build-up of fat inside the liver cells. It leads to an enlarged liver. It’s the most common alcohol-induced liver problem.
- Alcoholic hepatitis: Alcoholic hepatitis is an acute inflammation of the liver. There is death of liver cells, often followed by permanent scarring.
- Alcoholic cirrhosis: Alcoholic cirrhosis is the destruction of normal liver tissue. It leaves scar tissue in place of the working liver tissue.
What are the Symptoms?
The most common sign is Jaundice, a condition in which skin & whites of the eyes turn yellow. Other symptoms include:
- Nausea & vomiting
- Abdominal pain or tenderness
- Tiredness & fatigue
- Loss of appetite
- Slight fever
What are the Causes?
Following are some of the factors that play a role in alcoholic hepatitis:
- When the body’s tries to break down alcohol it produces highly toxic chemicals
- These chemicals lead to inflammation which damages the liver cells.
- Over a period of time, the healthy liver tissue gets replaced by scars which interfere with the liver function.
Other Factors that lead to Alcoholic hepatitis are:
- Consuming Alcohol with Hepatitis C
- Most heavy drinkers are malnourished as they eat less or their body’s do not absorb nutrients properly. This could be a contributing factor to cell damage in the liver.
How is it Diagnosed?
Your healthcare provider will do a complete health history and physical exam. Other tests used to diagnose alcohol-induced liver disease may include:
- Blood tests: Including liver function tests, which show whether the liver is working the way it should.
- Liver biopsy: This involves removing small tissue samples from the liver with a needle or during surgery. These samples are checked under a microscope to find out the type of liver disease.
- Ultrasound: This test uses high frequency sound waves to create a picture of the organs.
- CT scan: This imaging test uses X-rays and a computer to produce images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays.
- MRI: MRI uses a magnetic field, radio frequency pulses, and a computer to make detailed pictures of internal body structures. Sometimes injecting dye into a vein is used to produce images of body parts. The dye helps show the liver and other organs in the abdomen (belly).
What are the Risk Factor?
The main risk factor is the amount of alcohol a person consumes. Although it is unknown how much alcohol puts you at risk of alcoholic liver disease, research indicates that patients with this disease have a history of consuming over 100 grams every day for many years.
However, alcoholic liver disease can occur in individuals who drink much less, but have other risk factors which include:
- Gender: Women tend to have higher risk of developing alcoholic liver disease compared to men
- Obesity: People who are are overweight and consume excessive alcohol have a higher chance of developing alcoholic liver disease
- Genetic Factors: Research indicates that alcoholic liver disease may also be hereditary.
- Binge Drinking: Men consuming more than 5 drinks and women consuming 4 or more within a span of two hours increasing risk of alcoholic liver disease manifold.
How is it Treated?
If you have alcoholic liver disease (ALD), the crucial first step is to abstain completely from consuming alcohol, as continued consumption will lead to further progression of the disease. All of the alcohol-related disorders will improve with the cessation of drinking.
Treatment includes:
- Alcohol Withdrawal Treatment
- Nutritional Support
- Liver Transplant
- Treating Complications of ALD