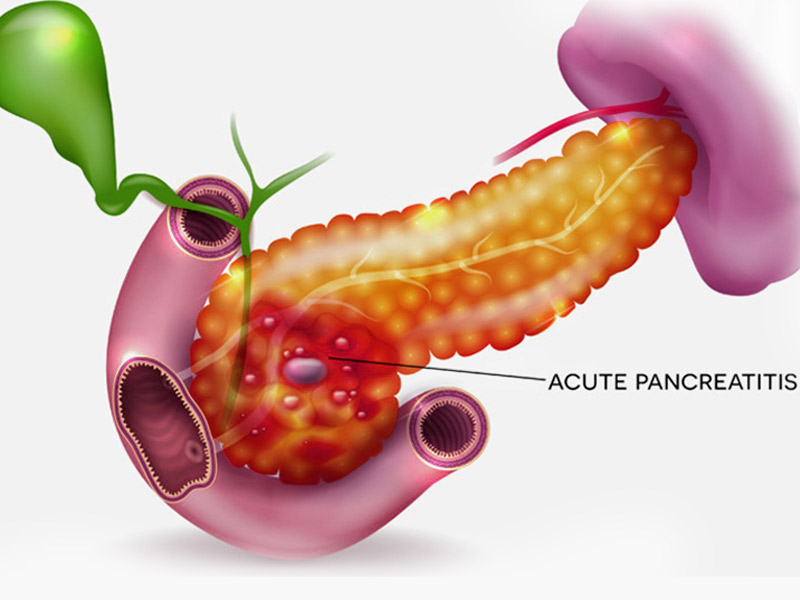
Acute pancreatitis
Acute pancreatitis is a condition where the pancreas becomes inflamed (swollen) over a short period of time. The pancreas is a small organ, located behind the stomach, that helps with digestion. Most people with acute pancreatitis start to feel better within about a week and have no further problems.
What are the Symptoms?
Pain in patients with acute pancreatitis is very mild initially but worsens quickly. It is constant, severe & can last for days in patients, if left untreated. Generally, patients with this disease look & feel very sick and need immediate medical help. In most cases, patient needs to be admitted to the hospital for at least 5 days.
Some of the common signs & symptoms of acute pancreatitis are
- Pain in the upper part of the abdomen
- Pain in the back
- Pain in the abdomen that tends to worsen after meals
- Mild Fever
- Nausea & Vomiting
- Tenderness in the abdomen
What are the Causes?
- Excessive Alcohol Consumption
- High Triglyceride Levels in Blood
- High Calcium levels in the blood
- Certain Medications
- Infections
- Autoimmune disorders
- Surgery
- Trauma
How is it Diagnosed?
To rightly diagnose acute pancreatitis, your doctor would need to understand your medical history, perform a physical examination and analyse your blood test results.
Following are some of the test that may be required to diagnose acute pancreatitis:
- Blood Tests to check for amylase & lipase levels
- Pancreatic Function Test
- Ultrasound
- CT Scan
- MRI
- ERCP
- Biopsy
What are the Risk Factor?
Factors that increase your risk of pancreatitis include:
- Excessive alcohol consumption: Research shows that heavy alcohol users (people who consume four to five drinks a day) are at increased risk of pancreatitis.
- Cigarette smoking: Smokers are on average three times more likely to develop chronic pancreatitis, compared with nonsmokers. The good news is quitting smoking decreases your risk by about half.
- Obesity: You’re more likely to get pancreatitis if you’re obese.
Diabetes. Having diabetes increases your risk of pancreatitis. - Family history of pancreatitis: The role of genetics is becoming increasingly recognized in chronic pancreatitis. If you have family members with the condition, your odds increase — especially when combined with other risk factors.
Pancreatitis can cause serious complications, including:
- Kidney failure: Acute pancreatitis may cause kidney failure, which can be treated with dialysis if the kidney failure is severe and persistent.
- Breathing problems: Acute pancreatitis can cause chemical changes in your body that affect your lung function, causing the level of oxygen in your blood to fall to dangerously low levels.
- Infection: Acute pancreatitis can make your pancreas vulnerable to bacteria and infection. Pancreatic infections are serious and require intensive treatment, such as surgery to remove the infected tissue.
- Pseudocyst: Acute pancreatitis can cause fluid and debris to collect in cystlike pockets in your pancreas. A large pseudocyst that ruptures can cause complications such as internal bleeding and infection.
- Malnutrition: Both acute and chronic pancreatitis can cause your pancreas to produce fewer of the enzymes that are needed to break down and process nutrients from the food you eat. This can lead to malnutrition, diarrhea and weight loss, even though you may be eating the same foods or the same amount of food.
- Diabetes: Damage to insulin-producing cells in your pancreas from chronic pancreatitis can lead to diabetes, a disease that affects the way your body uses blood sugar.
- Pancreatic cancer: Long-standing inflammation in your pancreas caused by chronic pancreatitis is a risk factor for developing pancreatic cancer.
How is it Treated?
Treatment for acute pancreatitis may include:
- Antibiotics
- Administering fluids intravenously to prevent dehydration
- Pain Medications
- Special Liquid Diet to ensure the patient get all the nutrients he or she needs
The underlying cause has to be addressed once the pain situation is under control. The following are some of the treatment methods that can help:
- ERCP or Endoscopic Retrograde Cholangiopancreatography is performed to remove gallstones if they are blocking the pancreatic or bile ducts
- Gallbladder Removal Surgery is generally performed within two weeks of confirming the diagnosis
- Pancreatic Surgery to remove the fluids or dead tissue