Achalasia Cardia
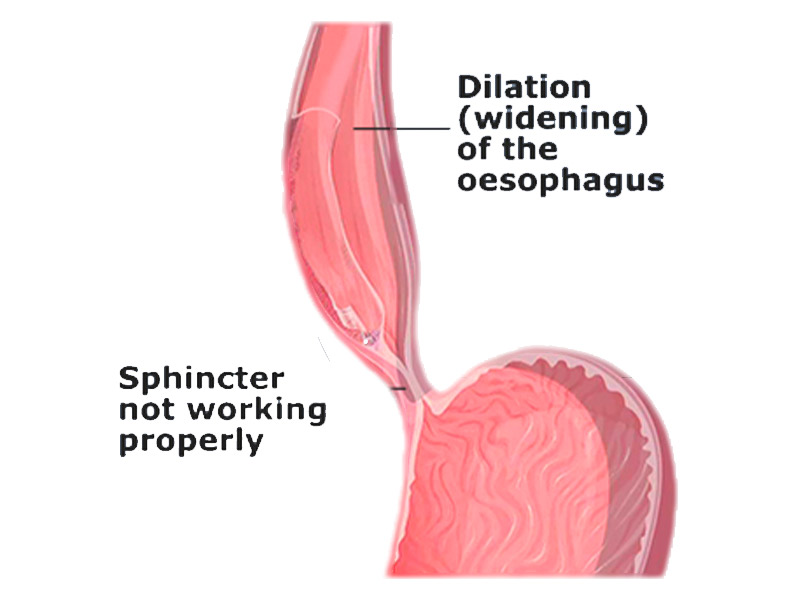
Achalasia is a rare digestive disorder that affects the nerves in the Esophagus. As a result, the lower Esophageal sphincter loses its ability to open, making it hard for food or liquid to pass into the stomach. The word Achalasia means “failure to relax”. Achalasia adversely impacts the coordinated muscular activity of the Esophagus that transports food from throat to stomach.
The Esophagus consists of both muscles & nerves. The nerves help in relaxation & opening of the sphincter. Achalasia impacts both nerves & muscles. During the initial phases of the disease, an inflammation occurs in the muscles around the nerves. As the disease advances, degeneration of nerves occurs & leads to their disappearance. This happens mostly in nerves that help the sphincter relax.
What are the Symptoms?
- Difficulty Swallowing Foods – both solid & liquid
- Discomfort in the chest due to retained food
- Regurgitation of food
- Pain in the chest
- Heartburn
- Loss of weight due to reduce food consumption
What are the Causes?
The exact cause of achalasia is poorly understood. Researchers suspect it may be caused by a loss of nerve cells in the esophagus. There are theories about what causes this, but viral infection or autoimmune responses have been suspected. Very rarely, achalasia may be caused by an inherited genetic disorder or infection.
How is it Diagnosed?
Achalasia can be overlooked or misdiagnosed because it has symptoms similar to other digestive disorders. To test for achalasia, your doctor is likely to recommend:
Esophageal manometry: This test measures the rhythmic muscle contractions in your esophagus when you swallow, the coordination and force exerted by the esophagus muscles, and how well your lower esophageal sphincter relaxes or opens during a swallow. This test is the most helpful when determining which type of motility problem you might have.
X-rays of your upper digestive system (esophagram): X-rays are taken after you drink a chalky liquid that coats and fills the inside lining of your digestive tract. The coating allows your doctor to see a silhouette of your esophagus, stomach and upper intestine. You may also be asked to swallow a barium pill that can help to show a blockage of the esophagus.
Upper endoscopy: Your doctor inserts a thin, flexible tube equipped with a light and camera (endoscope) down your throat, to examine the inside of your esophagus and stomach. Endoscopy can be used to define a partial blockage of the esophagus if your symptoms or results of a barium study indicate that possibility. Endoscopy can also be used to collect a sample of tissue (biopsy) to be tested for complications of reflux such as Barrett’s esophagus.
What are the Risk Factor?
Some complications of achalasia are the result of food backing up (regurgitating) into your esophagus and then drawn into (aspirated) your trachea (windpipe), which leads to your lungs.
These complications include:
- Pneumonia.
- Lung infections (pulmonary infections).
Other complications include:
- Esophageal cancer: Having achalasia increases your risk of this cancer.
How is it Treated?
Treatment for Achalasia is focused on relaxing or forcing open the sphincter so that food & liquid can move more easily through the digestive system. There are two treatment modalities for Achalasia – Surgical & Non Surgical.
Nonsurgical Treatment options include:
- Pneumatic Dilation: This procedure involves insertion of a balloon into the Esophagus & inflation to enlarge the opening.
- Botox or Botulinum toxin type A: Botox is a muscle relaxant that is directly injected into the sphincter with the help of an endoscope.
- Medication: Certain muscle relaxants may be recommended for patients who aren’t suited for any of the other treatment options.
Surgical Treatment options include:
- Heller myotomy: In this procedure, the muscle at the lower end of the Esophageal sphincter to allow food & liquids to pass more easily into the stomach.
- Fundoplication: In this procedure, the top part of the stomach is wrapped around the lower Esophageal sphincter to tighten the muscle & prevent acid reflux.
- Peroral Endoscopic Myotomy (POEM): This is a surgical procedure in which an incision is made in the inner lining of the Esophagus through an endoscope. After an incision is made, the doctor then cuts the muscle at the lower Esophageal sphincter just as in heller myotomy