Celiac Disease
Celiac disease, sometimes called celiac sprue or gluten-sensitive enteropathy, is an immune reaction to eating gluten, a protein found in wheat, barley and rye.
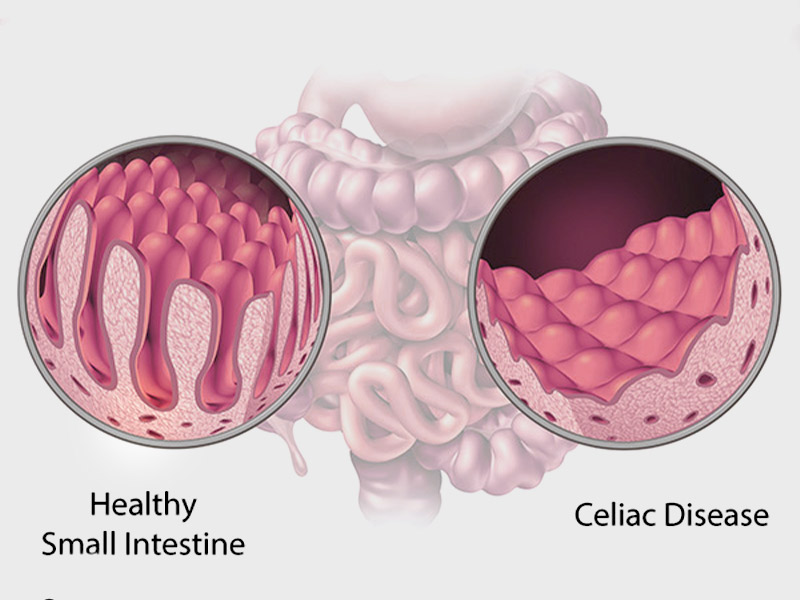
If you have celiac disease, eating gluten triggers an immune response in your small intestine. Over time, this reaction damages your small intestine’s lining and prevents it from absorbing some nutrients (malabsorption).
What are the Symptoms?
If a person has celiac disease & eats gluten, he or she may experience the following symptoms:
- Pain in the abdomen
- Constipation or Diarrhea
- Heartburn
- Bloating
- Anemia
- Vomiting
- Weight Loss
- Foul Smelling stool
- Fluid Retention
- Pale sores in the mouth
- Tooth Discolouration
- Numb hands or feet
Children with this medical disorder tend to present the following symptoms:
- Bloating
- Constipation
- Diarrhea
- Upset stomach or vomiting
- Weight loss
What are the Causes?
- Your genes combined with eating foods with gluten and other factors can contribute to celiac disease, but the precise cause isn’t known.
- Infant-feeding practices, gastrointestinal infections and gut bacteria might contribute, as well.
- Sometimes celiac disease becomes active after surgery, pregnancy, childbirth, viral infection or severe emotional stress.
- When the body’s immune system overreacts to gluten in food, the reaction damages the tiny, hairlike projections (villi) that line the small intestine.
- Villi absorb vitamins, minerals and other nutrients from the food you eat. If your villi are damaged, you can’t get enough nutrients, no matter how much you eat.
How is it Diagnosed?
Common Blood tests to diagnose Coeliac Disease:
- Complete Blood Count
- Liver Function Test
- Cholesterol Test
- Serum Albumin Test
- Alkaline Phosphatase Level Test
The blood tests have to be conducted before going gluten-free as eliminating gluten from your diet before diagnosis might not give accurate results.
If the results of these tests indicate celiac disease, your doctor will likely order one of the following tests:
- Endoscopy. This test uses a long tube with a tiny camera that’s put into your mouth and passed down your throat (upper endoscopy). The camera enables your doctor to view your small intestine and take a small tissue sample (biopsy) to analyze for damage to the villi.
- Capsule endoscopy. This test uses a tiny wireless camera to take pictures of your entire small intestine. The camera sits inside a vitamin-sized capsule, which you swallow. As the capsule travels through your digestive tract, the camera takes thousands of pictures that are transmitted to a recorder.
What are the Risk Factor?
Risk of getting this disease is higher in individuals with certain medical conditions:
- Addison’s disease
- Down syndrome
- Rheumatoid Arthritis
- Turner syndrome
- Type 1 diabetes
Coeliac disease can have serious complications if untreated.
- Cancer
- Damaged tooth enamel
- Infertility & miscarriage
- Lactose Intolerance
- Malnutrition
- Seizures
- Numbness in hands & feet
- Pancreatic Disease
How is it Treated?
There are no medications that can treat Coeliac disease. The only way to manage it is to follow a lifelong gluten free diet. This helps the intestinal villi to heal itself & absorb the nutrients properly.
For most people with celiac disease, a gluten-free diet will allow the small intestine to heal. For children, that usually takes three to six months. For adults, complete healing might take several years.
If you continue to have symptoms or if symptoms recur, you might need an endoscopy with biopsies to determine whether your intestine has healed.
If your small intestine is severely damaged or you have refractory celiac disease, your doctor might recommend steroids to control inflammation. Steroids can ease severe signs and symptoms of celiac disease while the intestine heals.